Epworth Sleepiness Scale Pdf Deutsch
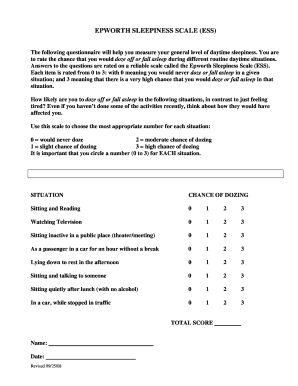
Medhat Kalliny MD, PhD, FAAFP, in, 2019 Epworth sleepiness scaleThe Epworth sleepiness scale (ESS) measures daytime sleepiness and consists of eight items (situations) where individuals assess how likely they would fall asleep. A sum of responses is calculated for a total score ranging from 0 to 24 with a total score ≥10 represents excessive daytime sleepiness. 104 To investigate the daytime sleepiness and hyperactivity secondary to obstructive sleep apnea in adolescents, the ESS was modified by Melendres et al. (2004) to make it more appropriate for use with adolescents.
Results supported the validity of the modified ESS where adolescents with sleep disordered breathing scored higher on the ESS than controls. 105 Moore et al. (2009) demonstrated that the ESS scores correlated with self-reports of anxiety and general health status. 106 However, no psychometrics for the ESS in adolescents or children have been established. Wynne Chen, Emmanuel Mignot, in, 2007 Epworth Sleepiness Scale (ESS)The Epworth Sleepiness Scale (ESS) is an eight-item, self-rating scale.
It assesses the patient's likelihood of falling asleep (dozing behavior) during the course of the day during eight, normal everyday situations of varying soporific nature (sitting, watching TV, in a car, talking to someone). The patient is asked to rate the likelihood of falling asleep on a scale from 0–3, where 0 indicates no chance of falling asleep or dozing, and 3 represents a very high chance of falling asleep. The total ESS score ranges from 0 to 24, with higher scores reflecting a greater sleep propensity. 60 A total score of 10 or more suggests pathologic sleepiness, requiring further evaluation and treatment.
18,61 Most patients with a complaint of excessive daytime sleepiness have scores of 12 or higher (for example, more than 90% of narcoleptic subjects have an ESS ≥ 12, personal data in over 1000 narcoleptic subjects). Of importance, however, many control subjects, approximately 25% of a general population sample, score high (≥12) on this scale.
High scores on the ESS also do not necessarily correlate well with MSLT mean sleep latencies. 62–64 A disconnection between the two may suggest fatigue rather than sleepiness, 65 a psychiatric hypersomnia, 66-68 or, in some cases, idiopathic hypersomnia. QUESTIONHYPOTHETICAL SITUATION TO BE RATED1Sitting and reading2Watching television3Sitting inactive in a public place (e.g., a theater or a meeting)4As a passenger in a car for an hour without a break5Lying down to rest in the afternoon when circumstances permit6Sitting and talking to someone7Sitting quietly after a lunch without alcohol8In a car, while stopped for a few minutes in trafficESS's popularity stems in part from its simplicity, brevity, and validation. Johns established reliability and validity using 54 patients with sleep apnea (before and after continuous positive airway pressure therapy) and 104 medical students. 32, 33 Student controls had a mean score of 7.6.
Patients with sleep apnea had a mean score of 14.3 at baseline that declined to 7.4 after treatment. In another study, normative values were gathered from 942 patients waiting at outpatient clinics (e.g., dermatology, audiology, and ophthalmology clinics) and 1120 healthy people attending health fairs or community health lectures. The mean ESS total score for these two groups were 8.1 and 5.2, respectively. 34 Based on this study and subsequent work in our clinic, we categorize ESS scores ranging from 0 to 8 as normal, 9 to 12 as mild, 13 to 16 as moderate, and greater than 16 (an order of magnitude above high normal) as severe.ESS differs from other tests in that respondents are not asked about how they feel but rather to make a probability judgment about their own behavior. In this manner, persons completing the ESS are indirectly rating their sleep drive and may explain why ESS correlates (albeit weakly) with MSLT sleep latency (an objective index of sleep drive). ESS's main disadvantage is its questionable utility when it is readministered within a brief time interval.
Its sensitivity to age, acute sleep disturbance or deprivation, and drugs needs further research. QuestionHypothetical Situation to Be Rated1Sitting and reading2Watching television3Sitting inactive in a public place (e.g., a theater or a meeting)4As a passenger in a car for an hour without a break5Lying down to rest in the afternoon when circumstances permit6Sitting and talking to someone7Sitting quietly after a lunch without alcohol8In a car, while stopped for a few minutes in trafficThe popularity of the ESS stems in part from its simplicity, brevity, and validation. Johns established reliability and validity using 54 patients with sleep apnea (before and after continuous positive airway pressure therapy) and 104 medical students.
3,4 Student control subjects had a mean score of 7.6, compared with 14.3 at baseline for patients with sleep apnea. After treatment, the mean score for patients with sleep apnea declined to 7.4. In another study, normative values were gathered from 942 patients waiting at outpatient clinics (e.g., dermatology, audiology, and ophthalmology clinics) and 1120 healthy people attending health fairs or community health lectures. The mean ESS total scores for these two groups were 8.1 and 5.2, respectively. 5 On the basis of this study and subsequent work in our clinic, we have categorized ESS scores ranging from 0 to 8 as normal, 9 to 12 as mild, 13 to 16 as moderate, and greater than 16 (double that of high normal) as severe.The ESS differs from other tests in that respondents are not asked about how they feel but rather to make a probability judgment about their own behavior.
Thus the ESS asks subjects to rate their own sleep drive; this may explain why ESS results correlate (albeit weakly) with Multiple Sleep Latency Test (MSLT)-determined sleep latency (an objective index of sleep drive). The ESS's main disadvantage is its questionable utility when it is readministered within a brief time interval. Maree Barnes, in, 2011 Subjective sleepinessThe Epworth Sleepiness Scale (ESS) is a simple, widely used subjective measure of sleepiness, which asks about the likelihood of falling asleep in a variety of situations ( Johns, 1991). Average scores of 9.5, 11.5, and 16.0 were recorded in patients with mild, moderate, and severe OSA from a clinic population, compared to 5.9 in a control group (potential range 0–24; Johns, 1991).
Moderate to severe sleepiness was found in a study of 54 patients with OHS, who had a mean ESS of 16 ( Perez de Llano et al., 2005). Increased sleepiness on the ESS has also been found in general population studies of OSA. In the Sleep Heart Health study, the mean ESS scores were 7.2, 7.8, 8.3, and 9.3 for subjects with normal polysomnography, mild, moderate, and severe OSA, respectively ( Gottlieb et al., 1999). The lesser sleepiness in the latter study may relate to the different study populations (clinic vs. General population). Other methods assessing the propensity to fall asleep in different situations have also identified increased sleepiness in OSA subjects. In the Wisconsin sleep cohort, subjects were described as excessively sleepy if they “woke unrefreshed regardless of how long they had slept,” “felt excessively sleepy during the day,” and had “uncontrollable daytime sleepiness that interfered with daytime living” at least 2 days a week.
Epworth Sleepiness Scale
Sixteen percent of men with OSA had all three symptoms compared to only 3% of men without OSA ( Young et al., 1993). The functional outcomes of sleep questionnaire (FOSQ) is a sleep-specific quality of life tool, with subscales related to activity level, vigilance, general productivity, social outcome, and intimate and sexual relationships ( Weaver et al., 1997).
Subjects with moderate OSA indicated significantly more difficulty with sleepiness on all subscales of the FOSQ and on the FOSQ global score. Increased sleepiness on both the ESS and FOSQ is related to elevated road crash risk ( Howard et al., 2004), thus signifying real-world relevance. QuestionHypothetical Situation to Be Rated1Sitting and reading2Watching television3Sitting and inactive in a public place (e.g., a theater or a meeting)4As a passenger in a car for an hour without a break5Lying down to rest in the afternoon when circumstances permit6Sitting and talking to someone7Sitting quietly after a lunch without alcohol8In a car, while stopped for a few minutes in trafficIt is worth noting that in situations 1, 3, 6, and 7, the subject is explicitly sitting; in situations 2, 4, and 8, the subject is presumably sitting; and in situation 5, the subject is lying down. ESS also differs from other tests in that respondents are not being asked to interpret their internal state but rather to make a judgment about their behavior. Furthermore, in a sense, individuals completing the ESS are rating their drive to sleep in probability projections. This may explain why the ESS has a small but statistically significant correlation with the MSLT, an objective index of sleep drive. Johns 44 45 conducted reliability and validity studies on 54 patients with sleep-related breathing disorders (before and after treatment with continuous positive airway pressure) and 104 medical student control subjects.

Student control subjects had a mean score of 7.6. Initially elevated scores (mean, 14.3) among patients with sleep-related breathing disorders declined to the normal range (mean, 7.4) after treatment. ESS scores increased as a function of increasing severity of their sleep-disordered breathing. 44 46 In another study, normative values were gathered from 942 patients waiting at outpatient clinics (e.g., dermatology, audiology, ophthalmology clinics) and 1120 healthy people attending health fairs or community health lectures.
The mean ESS total score for these two groups were 8.1 and 5.2, respectively. 47 Considering an order of magnitude above the mean as profound sleepiness, we categorize ESS 0 to 8 as normal, 9 to 12 as mild, 13 to 16 as moderate, and greater than 16 as severe.The popularity of ESS stems in part from its simplicity and brevity. This, in conjunction with the validation studies, has made it perhaps the most commonly administered self-report scale for daytime sleepiness.
One disadvantage is the questionable usefulness of the test when readministered within a brief time interval; consequently, it is not useful for evaluating circadian rhythm influences on sleepiness. In addition, the sensitivity to age, acute sleep disturbance or deprivation, and drugs is not known. For older children, a modified Epworth Sleepiness Scale (ESS) with the last item “chance of dozing in a car while stopped for a few minutes in traffic” replaced by “doing homework or taking a test.” The question about sitting quietly after lunch has “without alcohol” removed. A four-item Pediatric Sleep Questionnaire (PSQ-SS) 2 has also been used ( Table F18-1).
Parents’ answers are obtained, but the physician is encouraged to ask the child for input. In one study, the test distinguished children with sleep-disordered breathing from controls.
1.Does your child wake up feeling unrefreshed in the morning? 2.Does your child have a problem with sleepiness during the day? 3.Does your child appears sleepy during the day according to comments of a teacher or other supervisor?
4.Is your child hard to wake up in the morning? Responses are Yes, No, or Don’t Know. If at least 2 of the 4 are positive, the child is classified as subjectively sleepy.From Chervin RD, Hedger KM, Dillon JE, Pituch KJ: Pediatric Sleep Questionnaire (PSQ): validity and reliability of scales for sleep-disordered breathing, snoring, sleepiness, and behavioral problems, Sleep Med 1:21-32, 2000. Mignot, in, 2017 Diagnostic ProceduresWhen evaluating patients with EDS, the Epworth Sleepiness Scale (ESS) is one of the most widely used, validated, subjective self-administered questionnaires. 8 When using this scale, patients rate their usual chances of dozing off or falling asleep in eight different daily situations on a 4-point scale (0–3). The total ESS score is the sum of the eight item-scores and can range between 0 and 24, with a higher score reflecting a higher level of daytime sleepiness.
It provides a subjective measure of an individual’s usual level of daytime sleepiness and sleep propensity in daily life. The ESS has not been validated in children, and the Pediatric Daytime Sleepiness Scale is more appropriate for use in this population. 46 In evaluating EDS, clinicians must differentiate sleepiness from fatigue and exhaustion, as patients often confuse the two. Fatigue presents as a lack of physical energy or body “tiredness.” The use of the Fatigue Severity Scale together with the ESS is often helpful in distinguishing EDS from fatigue. 47Several tests have been designed to objectively evaluate sleepiness. The multiple sleep latency test (MSLT) was first developed by Carskadon and Dement in 1977. 48 It was designed to measure physiologic sleep tendencies in the absence of external alerting factors.
The MSLT consists of a series of four to five napping tests conducted during the day and performed at 2 h intervals. To obtain a clinically valid MSLT, the test must be conducted under specific conditions. 49 First, it is recommended that patients keep a regular sleep schedule, allowing for adequate sleep in the days leading up to the test. To ensure this, patients are often asked to complete a sleep diary or to wear a wrist actigraphy for 2 weeks prior to the MSLT. Second, patients are asked to withhold taking medications such as sedatives, stimulants, and those that affect the propensity to enter REM sleep, particularly tricyclic antidepressants and SSRIs/SNRIs, for 1–2 weeks prior to testing. Interrupting therapy too close to the test may also affect the results by creating rebound sleepiness or REM sleep. A drug screen should be performed on the morning of the test.
Third, a polysomnography (PSG) study must be performed on the night preceding the MSLT test. The PSG serves to evaluate for alternative and coexisting causes of chronic daytime sleepiness, such as undiagnosed obstructive sleep apnea. It is also used to keep track of the patients’ total sleep time; ideally at least 360 min of sleep must be observed to exclude inadequate sleep as a confounder. 50 Finally, the PSG is useful as patients with narcolepsy may have sleep onset REM periods (SOREMPs)—REM sleep which occurs within the first 15 min of sleep onset. During PSG and MSLT testing, the patient is monitored in a comfortable, soundproof, and dark bedroom. During the MSLT, patients are asked to stay awake between each nap. The initial nap opportunity begins 1.5–3 h after termination of nocturnal PSG, which ideally occurs at the patient’s usual wake up time.
Prior to each nap, the patient is instructed to lie quietly and attempt to fall asleep. The MSLT records the latency for each 4–5 min nap opportunity (time between lights out and sleep onset). If no sleep is observed for 20 min, then the nap ends. If the patient falls asleep, then the nap continues for another 15 min to evaluate for the possibility of a SOREMP. At the end of the test, the mean sleep latency (MSL) is calculated for all naps.
A MSL of 10–20 min is generally seen in healthy, rested subjects, while a MSL ≤ 8 min indicates sleepiness. This cut off is used for the diagnosis of both narcolepsy and IH, although ∼22% of the general population meets this criteria, and thus is not a very specific finding. 51 More importantly, in narcolepsy, patients generally exhibit multiple SOREMPs during the test, with at least two instances during nocturnal sleep onset and daytime naps considered diagnostic for the condition ( Fig. 8.5). Whereas a MSL ≤ 8 min is not a very specific finding, MSL ≤ 8 min and the observation of ≥ 2 SOREMPs is only found in approximately 2–4% of the population.
MSLT and PSG result from a narcolepsy type 1 patient.(Top) A PSG performed the night prior to the MSLT with a SOREMP (REM sleep occurs in the first 15 min of sleep)—a common finding seen in patients with narcolepsy type 1. (Middle panels) Continuous two 30 s epochs from a MSLT recording of a narcoleptic patient showing an abrupt transition from wake to REM sleep. (Bottom) A summary report of a MSLT from a patient with a mean sleep latency of 0.4 min across five naps and five out of five recorded SOREMPs.The PSG-MSLT has several limitations. While it has been validated in the context of Na-1, its use in diagnosis of Na-2 and IH have mostly been based on consensus and by extension. Clinicians should be mindful of the fact that SOREMPs are common in shift workers and can occur in other disorders that increase pressure for REM sleep, such as in insufficient sleep, untreated sleep apnea, or delayed sleep phase syndrome. It must also be performed free of any neuroactive substances, which is often difficult for patients with psychiatric or pain disorders. Further, whereas a positive MSLT in the context of Na-1 is reliable, repeatability in the context of Na-2 or IH is extremely poor.
52,53 Because there are no clear clinical differentiating features between IH and Na-2, 54 the two disorders are likely best considered as a spectrum and they should be treated similarly.Another polysomnographic test which can be used in the evaluation of EDS is the maintenance of wakefulness test (MWT). 55 As the name implies, the MWT assesses one’s ability to maintain wakefulness.
It was developed based on the assumption that the volitional ability to remain awake provides important information regarding one’s ability to do so. The MWT is conducted during the day and a variety of protocols have been used. The recommended protocol consists of four 40 min trials performed at 2 h intervals, with the first trial beginning at 1.5–3 h after the patient’s usual wake up time. Patients are instructed to maintain wakefulness while sitting comfortably in bed in a dark room. In normal controls, the mean sleep latency (to the first epoch of sleep) in a MWT was found to be at 30.4 ± 11.2 min, and a MSL ≤ 8.0 min is considered abnormal. 50 The MWT can be a useful tool in pharmacologic trials in evaluating response to a treatment for EDS, and in evaluating the risk of falling asleep associated with specific jobs or activities.A seldom-used test to document sleepiness is the continuous 24 or 36 h PSG.
This test aims to obtain information about the frequency, timing and duration of daytime sleep episodes, as well as documenting nighttime sleep disruptions. This test is typically performed using ambulatory equipment. Although the test is excellent in distinguishing Na-1 from other pathology and gives detailed information on the nature of each patient’s hypersomnia, it is difficult to perform and thus rarely used. The long polysomnographic recording may capture an episode of cataplexy in the evaluation of a narcolepsy by showing the absence of chin and muscle twitches in the awake patient. Moreover, a 24 h PSG can also be used to help evaluate patients who are suspected to have IH or Kleine–Levin syndrome (KLS) while they are experiencing an episode of hypersomnia.
Epworth Sleepiness Scale Pdf Spanish
Questionnaires such as the Stanford Sleepiness Scale or the Epworth Sleepiness Scale (ESS) 1 are measures of self-rated symptoms of sleepiness. The Stanford Sleepiness Scale ( Table F17–1) measures subjective feelings of sleepiness (“fogginess, beginning to lose interest in staying awake”). A score above 3 is considered “sleepy.” In contrast, the ESS measures self-rated average sleep propensity (chance of dozing) over eight common situations that almost everyone encounters. The propensity to fall asleep is rated as 0, 1, 2, or 3, where 0 corresponds to “never” and 3 to “a high chance of dozing” ( Table F17–2). The maximum score is 24, and normal is assumed to be 10 or less. ESS scores of 16 or greater are associated with severe sleepiness. Questionnaires such as the Stanford Sleepiness Scale or the Epworth Sleepiness Scale (ESS) 1,2 are measures of self-rated symptoms of sleepiness.
The Stanford Sleepiness Scale ( Table 14–1) measures subjective feelings of sleepiness (“fogginess, beginning to lose interest in staying awake”). A score above 3 is considered sleepy. In contrast, the ESS measures self-rated average sleep propensity (chance of dozing) over eight common situations that almost everyone encounters.
The propensity to fall asleep is rated as 0, 1, 2, or 3 where 0 corresponds to never and 3 to a high chance of dozing ( Table 14–2). The maximum score is 24 and normal is assumed to be 10 or less. ESS scores of 16 or greater are associated with severe sleepiness. SITUATION: “USUAL WAY OF LIFE IN RECENT TIMES”CHANCE OF DOZING SCORE 0, 1, 2, 3.Sitting and reading0–3Watching TV0–3Sitting, inactive in a public place (e.g., a theater or a meeting)0–3As a passenger in a car for an hour without a break0–3Lying down to rest in the afternoon when circumstances permit0–3Sitting talking to someone0–3Sitting quietly after a lunch without alcohol0–3In a car, while stopped for a few minutes in traffic0–3Total0–24.0 = would NEVER doze1 = SLIGHT chance of dozing2 = MODERATE chance of dozing3 = HIGH chance of dozing0–10 normal. The ESS correlates roughly with the severity of OSA (apnea-hypopnea index AHI) ( Table 14–3) 2,3 and improves (lower score) after continuous positive airway pressure (CPAP) treatment.
4 However, as noted in Table 14–3, there is a wide range of ESS scores at any level of OSA severity. A large study by Gottlieb and coworkers 3 found a modest correlation between the ESS and OSA severity in a large population-based study of 1824 subjects.
The degree of daytime sleepiness in the population was relatively mild ( Fig. Johns 2 reported a significant negative correlation between the ESS and the mean sleep latency (MSL) on the multiple sleep latency test (MSLT; an objective measure of sleepiness discussed in the next section) in a group of sleepy patients. However, Benbadis and colleagues 5 found no correlation between the MSLT findings and the ESS. Sangal and associates 6 found a statistically significant but low negative correlation between the ESS and the sleep latency (higher ESS associated with lower sleep latency) on the maintenance of wakefulness test (MWT) and MSLT in a large group of narcolepsy patients.
A scatter plot of ESS versus sleep latency on the MSLT is shown in Figure 14–2. There was also a modest correlation between the sleep latencies as determined by the MSLT and MWT. Of interest, the correlation between the MSLT and the MWT latencies (r = 0.52, P.